“Our Patients Come First.”
Sinus & Sinusitis in Baltimore, MD
Our goal at the Maryland ENT is to offer high-quality treatment to our patients. We focus on medical and surgical rhinology and related disciplines for both adults and children. Some of our medical treatments include:
- Nose ailments
- Sinus disorders
- Olfactory disorders
- Nasal allergy
- Functional nasal surgery for nasal obstruction
- Minimally invasive endoscopic sinus surgier
- Balloon sinuplasty
- Cosmetic nasal surgery
The physicians at Maryland ENT are known for their work in and Rhinology, nationally and internationally. Rhinology, Greek for “rhinos” or “nose”, is the study of the nose and sinuses. Rhinology handles all medical and surgical diseases of the nasal passages as well as paranasal sinuses.
About Our Physicians
The physicians of the Maryland ENT, inlcuding Dr Gol, have published numerous articles and publications in peer review journals and books, and made numerous presentations in national and international meetings, including the American Academy of Otolaryngology national meetings and specialty rhinology meetings in the US and around the world.
What is Balloon Sinuplasty?
Sinus Symptoms
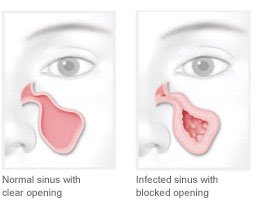
Sinusitis (also called rhinosinusitis) is an inflammation of the sinus lining that prevents normal mucus drainage through the nose. This blockage causes mucus to build up in the sinuses and can lead to very uncomfortable symptoms. Sinusitis symptoms may include:
- Sinus pressure and congestion
- Sinus Headache
- Facial pain
- Tenderness and swelling around the eyes, cheeks, nose and forehead
- Difficulty breathing through the nose
- Loss of the sense of smell or taste
- Yellow or green mucus from the nose
- Teeth pain
- Fatigue
- Sore throat from nasal discharge
- Bad breath
Balloon Sinuplasty In-Office
Office-based sinus dilation may be a compelling option for patients who decline or are ineligible for traditional OR-based surgery. With Balloon Sinuplasty In-Office, the majority of patients return to normal activity within two days of the procedure.
Balloon Sinuplasty In-Office – Clinical Benefits to an Expanded Patient Population
- Restore normal sinus drainage and function without bone or tissue removal, which preserves future treatment options
- Consider the opportunity for earlier intervention when medical therapy has failed
- Perform Balloon Sinuplasty In-Office procedures within a comfortable office setting under local anesthetic
- Lower the financial burden for eligible patients (reduced copay and procedural costs)
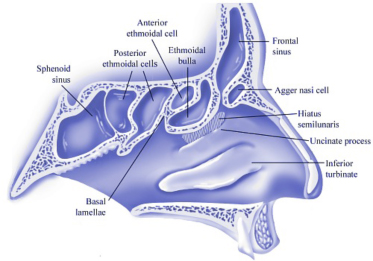
The paranasal sinuses are a group of four paired air-filled spaces that surround the nasal cavity (maxillary sinuses), above and between the eyes (ethmoid sinuses and frontal sinuses), and behind the ethmoids (sphenoid sinuses). The sinuses are named for the facial bones behind which they are located. Humans possess a number of paranasal sinuses, divided into subgroups that are named according to the bones within which the sinuses lie:
- the maxillary sinuses, are the largest of the paranasal sinuses, are under the eyes, in the maxillary bones.
- the frontal sinuses, superior to the eyes, in the frontal bone, which forms the hard part of the forehead.
- the ethmoid sinuses, which are formed from several discrete air cells within the ethmoid bone between the nose and the eyes.
- the sphenoid sinuses, in the sphenoid bone at the center of the skull base under the pituitary gland.
The pictures below show the sinus anatomy, detailing the frontal, ethmoid, and sphenoid sinuses.
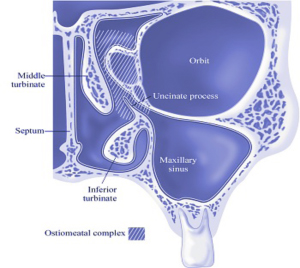
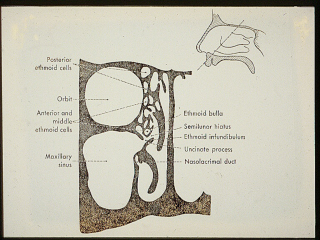
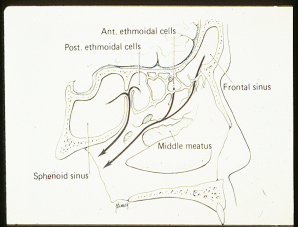
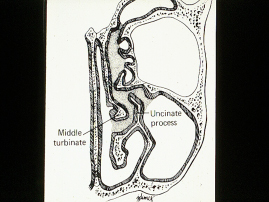
Blockage of the small sinus openings from swelling, infection, allergy, and other causes can result in sinusitis. The ostiomeatal complex is the most important sinus opening. Any process that causes blockage in this sensitive area can occlude the other sinuses that drain into the ostiomeatal complex.
When obstruction occurs, the mucus is retained in the sinus cavity, providing a medium for bacterial growth. Obstruction also leads to decreased oxygen levels within the sinus, which exacerbates sinus infections from both aerobic and anaerobic bacteria. These changes lead to damage to the sinus lining, leading to further tissue inflammation, which in turn leads to further blockage. These events demonstrate a vicious cycle that leads to chronic sinusitis.
Sinus FAQs
We have 2 frontal sinuses which are basically behind the brows and the forehead, 2 maxillary or cheek sinuses, 2 ethmoids sinuses which are located between the eyes and finally one sphenoid sinus which is deeper in the back of the nose closer to the brain.
We all have 3 to 4 turbinates in each side of the nose. These are structures inside of the nose that behave like sponges full of blood. They help warming the air we breathe and act as filters for all the particles that are present in the air we breathe. They swell in reaction to many things (allergy, infection, emotions…) creating the feeling of being congested.
Sometimes, the turbinate’s fail to shrink ( or decongest) creating a constant feeling of having the nose blocked. Medications and surgeries and help reduce the size of the turbinate’s and improve your breathing.
It is one of the most commonly diagnosed chronic illnesses in the United States, more prevalent than heart disease and migraine headaches. More than thirty-five million adult Americans suffered from it. If you have facial pain, nasal congestion, drainage, or post nasal drip for longer than three months, you may have chronic sinusitis.
Symptoms include headache, facial, pain/pressure, facial congestion/fullness, nasal obstruction/blockage, nasal discharge/purulence/discolored nasal drainage, hyposmia/anosmia (decreased smell), purulence in nasal cavity on examination, ear pressure/fullness, fever, halitosis, fatigue, dental pain, cough.
A number of symptoms can occur during a sinus infection. If you are experiencing one of these symptoms you are most likely suffering from sinusitis: pain and pressure, difficulty breathing and congestion, and postnasal drip.
The pain’s location relates sometimes to the infected sinus:
- Frontal sinusitis causes forehead pain or headache.
- Maxillary sinusitis causes cheek pain, which may radiate to the teeth in the upper jaw.
- Ethmoid sinusitis causes pain between the eyes or across the bridge of the nose.
- Sphenoid sinusitis causes pain behind the eyes, on the top of the scalp, or along the back of the head.
Difficulty breathing and congestion are one of the most common complaints in a sinus clinic. The most common reason for this congestion is a common cold because the inside of your nose is all swollen and full of mucus.
Allergies can also cause your nose to be congested during long period of times. Allergy symptoms can be controlled by medical treatment and less frequently by surgery to reduce the size of your turbinates.
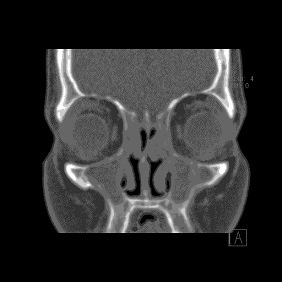
A common cause of nasal blockage is also septal deviation which means that the cartilage that separates the nose into a right and left passage is not straight causing a blockage in either side. The treatment of this condition is most of the times surgical. More rarely, nasal congestion can be caused by polyps in the nose or even a tumor. Diagnosis is usually made on endoscopy and on a CAT-scan of the nose and treatment is mainly surgical.
Mucus from the sinuses normally drains in the nose and down the back of the throat before being swallowed. If you have sinusitis, increased secretion by the nose and sinuses results in a larger volume of mucus, which is often thick and yellow or green making us more conscious of this phenomenon.
Symptoms such as itchy eyes, sneezing, and thin postnasal drip are likely due to allergies. You can be tested for allergies to determine what causes allergies to flare up. Finding the culprit help you avoid it. Your doctor can also desensitize you to this special agent reducing the need for allergy medications.
The roof of the nasal cavity is lined with special receptors to detect odor molecules that we breathe in. Losing sense of smell can be caused by an obstruction of the nose (congestion, infection such as the common cold) or even damage of these receptors by a viral infection, trauma, surgery, or even by an obstruction of the nose by polyps or tumors. Sometimes strokes can cause you to lose your sense of smell.
Most of the people who complain of a loss of taste usually have a loss of smell (like when you have a cold). In rare cases, the problem can be coming from the tongue or what is called the taste buds or even from the brain.
When mucus runs down the back of the throat, it may touch the vocal cords and trigger an involuntary cough response. Sinusitis is sometimes incriminated in persistent cough but other problems and lung infections and reflux need to be ruled out first.
Sinusitis may block the Eustachian tubes, passageways that connect your ears to the back of your nose. Their function is to equalize pressure between the inside of the ears (or middle ear space) and the outside atmosphere. This can explain why you feel like your ears are full when you are having a sinus infection.
While most of the acute sinus infections or acute sinusitis will cause some kind of low-grade fever, some will not.
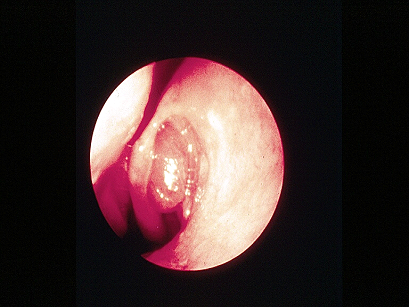
Your ENT physician at the Maryland ENT will perform a physical examination that includes nasal endoscopy using a state-of-the-art sinus endoscope that illuminates the depth of the nasal cavities and allows a clear and direct visualization of sinus pathology.
Your doctor may order a computed tomography (CT) scan to confirm the diagnosis. It is a radiological technique that uses a series of thin slices of x-ray pictures of the head and sinuses. A CAT scan typically takes 10 minutes to complete and in most cases can be done without the injection of an IV dye. CAT scan is very useful to diagnose and follow up long-standing sinus problems. CAT scans also help the surgeon planning a safe surgery avoiding critical structures like the brain and the eyes.
On a CAT scan, air is black and bone is white. Gray represents soft tissues and can signify disease (pus, inflamed mucosa, polyps).
Polyps are small growths attached to the sinus walls and made of inflamed and distorted sinus mucosa. Their precise cause is unknown but they usually occur in severe chronic infection of the sinuses. Their treatment is surgical when they obstruct the nose causing blockage, infection or loss of smell. They also tend to recur.
Treatment is almost never exclusively surgical. While surgery can help ventilate and drain the sinus, medical treatment plays a critical role in the healing process and in maintaining healthy sinus cavities.
Medical treatment includes but is not limited to oral antibiotics, nasal sprays, nasal saline rinses, oral steroids as well as topical antibiotics either in the form of a drug-eluting gel or a nebulized steroids or antibiotics.
A nebulizer can deliver medications such as antibiotics in high concentrations directly into the sinuses, where they can be most effectivesometimes sparing the need for oral treatment.
For a comprehensive review on how to treat sinusitis, please refer to this article on Medscape: Sinusitis: A Head and Neck Surgeon’s Perspective.
After asking you some questions about your general health and your symptoms, the doctor will perform a physical exam which may encompass most of the times an exam of your ears, your mouth and throat, your face and your neck.
Then, your doctor will most likely do a nasal endoscopy. He’ll first spray your nasal passages with a topical numbing medicine to reduce the tickle sensation and prevents you from sneezing.
Endoscopy helps your doctor see if the mucous membranes are inflamed if you are draining pus, if the turbinates are enlarged, if polyps are blocking the sinuses.
After making the correct diagnosis, your doctor will treat your condition accordingly. If you have sinusitis, he will prescribe an antibiotic and a nasal spray. If symptoms persist, the treatment can be repeated, with different medications. Typically, if the condition persists more than 3 months it becomes known as chronic rhinosinusitis, and some type of surgical intervention may be warranted.
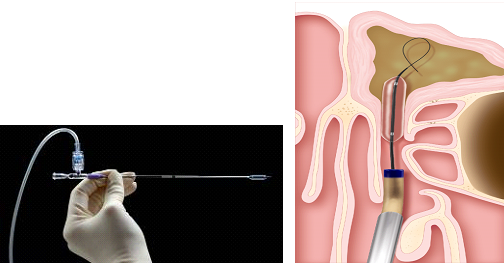
Balloon sinuplasty is an endoscopic surgical procedure for the treatment of blocked nasal sinuses. Patients diagnosed with chronic sinusitis but not responding well to medications may be candidates for balloon sinuplasty. Balloon sinuplasty technology was developed by Acclarent, Inc., and was brought to market in 2005, after FDA approval.
Balloon sinuplasty uses a small, flexible balloon catheter to enlarge sinus passageways. When the balloon is inflated, it widens the walls of the sinus passageway, with the goal of restoring normal sinus drainage without damaging the sinus lining.
Sinus surgery with Balloon Sinuplasty may be performed safely in a hospital, in an outpatient surgery center (under general anesthesia), or in a doctor’s office (under local anesthesia). The surgeon and patient will determine whether the procedure is best done under traditional general anesthesia or local anesthesia depending upon the patient’s medical history and the type of sinus disease that needs to be managed.
When performing Balloon sinuplasty, the physician inserts a sinus guide catheter through the nostril to gain access to the sinus ostia (openings) under endoscopic visualization. The endoscope allows the physician to see through the nasal passages to the sinus cavities to ensure that he/she is inserting the catheter into the proper location. A sinus guide wire or sinus illumination system is then introduced into the targeted sinus via the sinus guide catheter. The sinus illumination system provides a targeted fiber optic light transmission that helps the physician place the sinus guide catheter in the correct place. When the Balloon Sinuplasty system was introduced in 2005, illuminated wires did not exist and surgeons confirmed the location of the wires with low level x-ray using fluoroscopy.
Once access to the intended location is confirmed by light or fluoroscopy, a balloon catheter is introduced into the sinus cavity over the sinus guide wire or sinus illumination system and positioned in the blocked ostium for inflation. Once the position has been confirmed visually, the balloon is inflated to unblock the narrow or blocked ostium. The balloon is then deflated and removed. Next, an irrigation catheter may be advanced over the sinus guide wire or sinus illumination system to flush out the sinus of any mucus or pus. Finally, the sinus irrigation catheter is removed from the sinus to allow the sinus cavity to drain any mucus and/or pus. Newer balloon catheters have the irrigation system incorporated into the balloon making the procedure simpler with fewer steps.
Endoscopic sinus surgery (ESS) came into existence because of pioneering work of Messerklinger and Stamberger (Graz, Austria, 1970’s). Other surgeons have made additional contributions (first performed in USA by Kennedy in 1985). It is done either under local or general anesthesia, depending on the extent of the procedure, and using an endoscope, disease and obstructing bone and polyps are removed from the nose and sinus cavities are opened. The physicians at the Maryland Nose and Sinus Center have performed several thousands of sinus surgeries over the last 20 years. In our hands, the success rates of primary endoscopic sinus surgeries are superior to 90%.
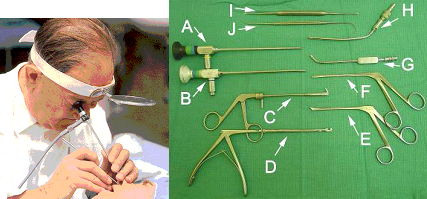
Recovery time is highly variable among individuals and according to the type and extent of surgeries. Balloon sinuplasty is now an in-office procedure that is under local anesthesia that usually does not require packing. Recovery is immediate and patients are back to work immediately. Endoscopic sinus surgery is an operating room procedure that usually requires packing. Packs are removed one week after surgery and nasal cavities are suctioned. By this time most of the patients would have resumed near-normal life.
In the immediate post-op period you should refrain from any vigorous physical activity which may increase the risk of bleeding. You will have antibiotics and pain medications, and you will be asked to rinse your nose with nasal saline.
Complications of sinus surgery are. Starting from the most common:
- Bleeding hence nasal packing helps prevent or control post-operative bleeding, infection. Bacteria multiply on crusts and old blood clots that are called debris.
- You will have antibiotics after surgery to prevent infection.
- You will also be scheduled for a debridement one week after surgery to remove all these crusts and help prevent complications.
- Religious nasal rinse routine can also help prevent infection and speed up the healing.
Very rare but serious complications are extremely rare and include the following:
- Spinal fluid leak: The bone making up the roof of your nose and separating your brain from your sinuses is thin can be breached during surgery creating what is called a cerebral spinal fluid (CSF) leak from the brain into the nose. If this leak persists, the patient risks developing meningitis. The breach, if identified, can be closed immediately at the time of surgery.
- Orbital hematoma/Decreased vision: Injury to the eye itself or to its muscles and nerves may leave patients with impaired vision, including double vision or blindness.
Bleeding after sinus surgery (epistaxis) is an uncommon occurrence. It came be minimized by meticulous surgical technique by the surgeon, thorough knowledge of the anatomy so that to avoid hitting any of the large arteries, and precise use of the surgical instruments during the procedure. Yu can help by avoiding any blood thinners (such as aspirin, ibuprofen, Plavix or Coumadin) immediately before the surgery. In case significant bleeding is encountered, this can be controlled by nasal packing.
When performed correctly, endoscopic sinus surgery (ESS) is highly effective for the treatment of chronic rhinosinusitis (CRS), with a 97-98% improvement in symptoms reported during the 12 months after surgery. However the outcome is affected not only by the skills of the surgeon, but also by certain factors that the patient controls (such as allergies, smoking and GERD or Gastro-Esophageal Reflux Disease). Even when FESS is performed by a good surgeon, long-term follow-up shows that the beneficial effects dissipate over time with gradual worsening of the sinusitis symptoms in 5-25% of patients after 3 years, and 3-14% of patients requiring revision ESS. Patients who continue to show clinical evidence of sinusitis, despite surgery and intensive medical treatment are labeled as having refractory CRS (or recalcitrant CRS) and often pose a therapeutic challenge to the treating rhinologist. For those frustratingly difficult sinus cases, he has developed a novel multi-factorial treatment protocol (called “Rhinotopic Therapy” protocol*), which includes topical nasal nebulization and a hydroxyl-ethyl cellulose biodegradable gel that releases antibiotics and corticosteroids inside the nasal cavity. Rhinotopic Therapy has proven effective in reversing mucosal changes and promoting healing of the mucosal surface epithelial barrier in refractory CRS.
Chahine KA, Alqudah MA. The rhinotopic protocol for chronic refractory rhinosinusitis: how we do it. Clin Otolaryngol. 2010 Aug;35(4):329-32. http://onlinelibrary.wiley.com/doi/10.1111/j.1749-4486.2010.02157.x/full
* Topical Membrane Therapy for Chronic Rhinosinusitis. Source: Peculiar Aspects of Rhinosinusitis. ISBN 978-953-307-763-5. Edited by: Gian Luigi Marseglia and Davide Paolo Caimmi. Published November 2011 http://www.intechopen.com/articles/show/title/topical-membrane-therapy-for-chronic-rhinosinusitis
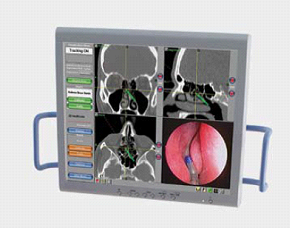
Image-guided surgery is a recent development that you may benefit from, particularly if you need an advanced surgical procedure done. It is a technological tool designed to help surgeons guide their instruments through the sinus cavities with millimeter accuracy while showing them exactly where they are in the nose on a monitor. This requires doing a preoperative sinus CAT scan, performed according to the machine protocol.
The surgical procedure to correct a deviated septum is called a septoplasty or nasal septum reconstruction, and is performed under general anesthesia. The surgeon makes an incision just inside the nostril, lifts the mucous membranes on the septum, and remodels or removes the portion of the cartilage and bone that’s deviated. Then the surgeon places dissolvable stitches or inserts nasal packing at the conclusion of the procedure. Complications are rare but may include bleeding, infection, perforation and over resection of the septum.
They can be shrunk with a radio-frequency needle by a process called radiofrequency coblation. This is a relatively new option which delivers a measured dose of electrical energy to heat and shrink swollen turbinate tissue. This procedure is usually done under local anesthesia. Alternatively, enlarged inferior turbinates can be remedied with a surgical procedure known as sub-mucous resection, in which a portion of the obstructing turbinate bone is removed with the patient under general anesthesia.
Pituitary adenomas are tumors that occur in the pituitary gland, and account for about 15% of intracranial neoplasms. Tumors which exceed 10 mm in size are defined as macroadenomas, and those smaller than 10 mm are referred to as microadenomas. Most pituitary adenomas are microadenomas, which often remain undiagnosed, and have an estimated prevalence of 16.7% (14.4% in autopsy studies and 22.5% in radiologic studies). Pituitary tumors are classified into secretive and non-secretive based on plasma hormone levels. Hormone secreting pituitary adenomas cause one of several forms of hyperpituitarism. The specifics depend on the type of hormone. Some tumors secrete more than one hormone, the most common combination being GH and prolactin. In addition, a pituitary adenoma may present with visual field defects, classically bitemporal hemianopia. It arises from the compression of the optic nerve by the tumor. The specific area of the visual pathway at which compression by these tumors occurs is at the optic chiasma. Also, a pituitary adenoma can cause symptoms of increased intracranial pressure. Prolactinomas often start to give symptoms especially during pregnancy, when the hormone progesterone increases the tumor’s growth rate. Headaches may be present.
Treatment options depend on the type of tumor and on its size:
- Prolactinomas are most often treated with bromocriptine or more recently, cabergoline or quinagolide which decrease tumor size as well as alleviates symptoms, both dopamine agonists, and followed by serial imaging to detect any increase in size. Treatment where the tumor is large can be with radiation therapy or surgery, and patients generally respond well.
- Somatotrophic adenomas respond to octreotide, a long-acting somatostatin analog, in many but not all cases according to a review of the medical literature. Unlike prolactinomas, thyrotrophic adenomas characteristically respond poorly to dopamine agonist treatment.[4]
- Surgery is a common treatment for pituitary tumors. Trans-sphenoidal adenectomy surgery can often remove the tumor without affecting other parts of the brain. Endoscopic surgery has become common recently.